How we’ve adapted our eye health work during the pandemic

“The impact of COVID-19 for people with sight loss in Africa and Asia is devastating,” explains Dr Kola Ogundimu, Sightsavers’ eye health senior global technical lead.
“While many have been unable to spend time with those closest to them, the pandemic has also prevented them from accessing life-changing eye care treatment.
“We know that across the world, 2.2 billion people have a visual impairment, but for at least one billion people it could have been prevented or can still be treated. It has been essential for us to not only restart our eye health programmes quickly and safely, to provide much needed diagnoses, glasses and surgeries, but also to work flexibly to respond to the ongoing health crisis and build back stronger healthcare for the future.”
Tiangay Gondoe, programme manager in Sierra Leone
“Life in Sierra Leone is difficult during these times. As well as the pandemic, prices of basic commodities have increased, making it difficult for the average Sierra Leonean.
“Although our eye health operations are still under review, my hopes are that operations will restart for patients with negative COVID-19 test results.
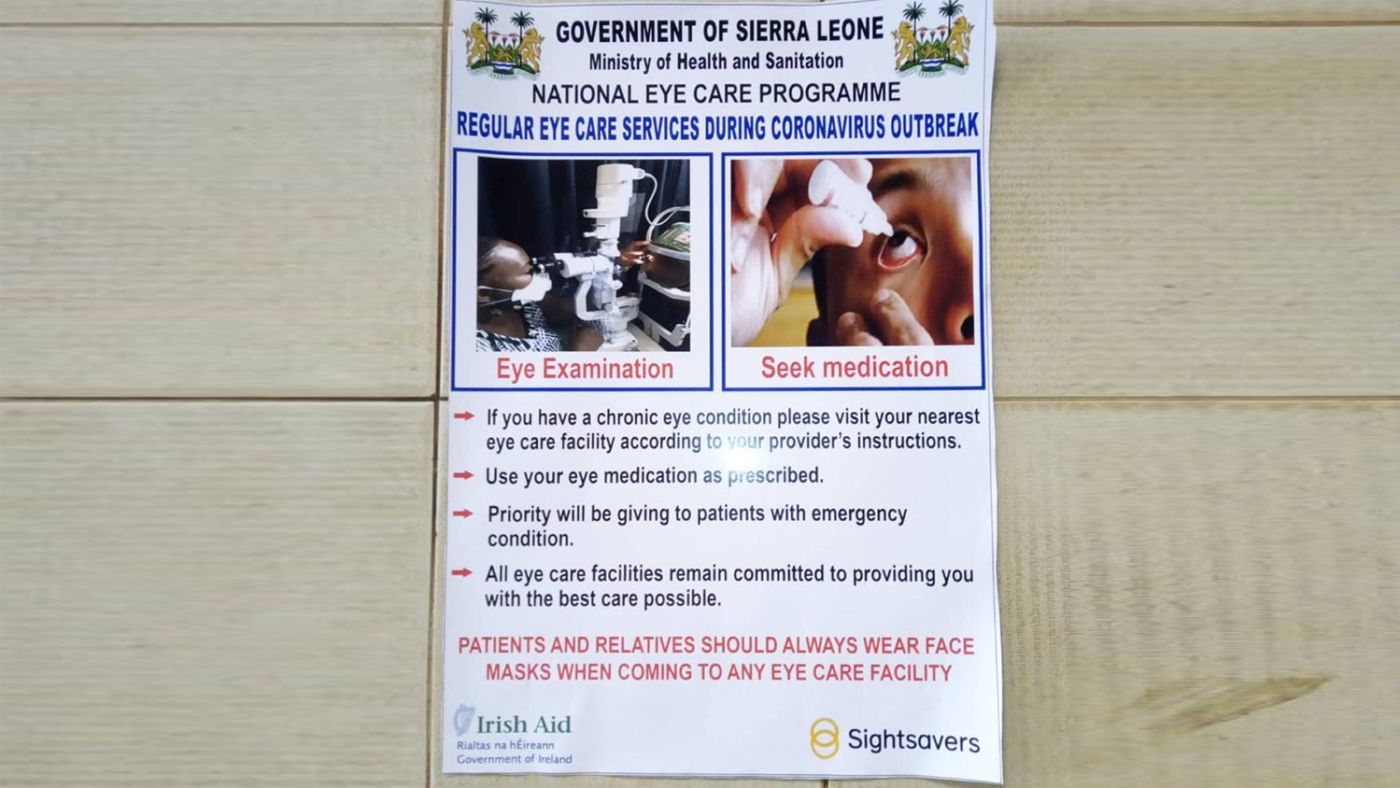
“We’re working with the government and the national eye health programme manager, and regional managers in eye departments within government hospitals, to train health workers on COVID-19 transmission, symptoms and the risks of carrying out treatment that requires close contact with patients.
“This training has led to eye health workers raising awareness and promoting preventative messages to an estimated 1,000 patients, including women, children, and people with disabilities. We’re also providing health workers with PPE and hygiene kits, and supporting eye health clinics to ensure staff and patients adhere to social distancing and hygiene measures.” More from Sierra Leone
Cristina Pires, programme officer in Mozambique
“COVID-19 cases are spreading fast, mostly in Cabo Delgado, the capital Maputo and Nampula province, but the public are still ignoring prevention measures announced by the authorities.
“I would like the eye health programme to recover from this sad situation. Prevention measures must be taken by eye health units and eye health staff, as well as patients, to ensure we can provide eye health services to all those in need. We’ve developed protocols to slowly reopen screening camps to identify people with cataracts. We have also developed a training module for community health workers, which will focus on how to restart camps safely.
“We’ve adapted our projects to ensure people with disabilities don’t get left behind in the COVID-19 response. We’re working with the Social Communication Institute to make sure people with disabilities receive information on COVID-19 in accessible formats. We’re developing COVID-19 awareness messages and are advertising these on the radio, and in the street by announcing through a megaphone from a car.
“Working with the Ministry of Gender, Child and Social Action, we’re helping to distribute basic food baskets and providing tippy tap buckets for hand washing. We’ve also purchased two sewing machines for tailors with disabilities so they can make face masks. About 1,000 masks have been made for people with disabilities in rural and remote communities in six districts.
“I hope that eye health continues to be accessible for everyone: women, men, girls and boys and particularly older people who haven’t seen their families for a long time.” More from Mozambique
David Agyemang, programme manager in Ghana
“Life is almost back to ‘normal’ in Ghana, athough all Ghana’s borders, except by air, are closed to human traffic. Internally, there are no restrictions on business, and public health activities are continuing. Face masks are mandatory, and handwashing and the use of hand sanitisers are being promoted.
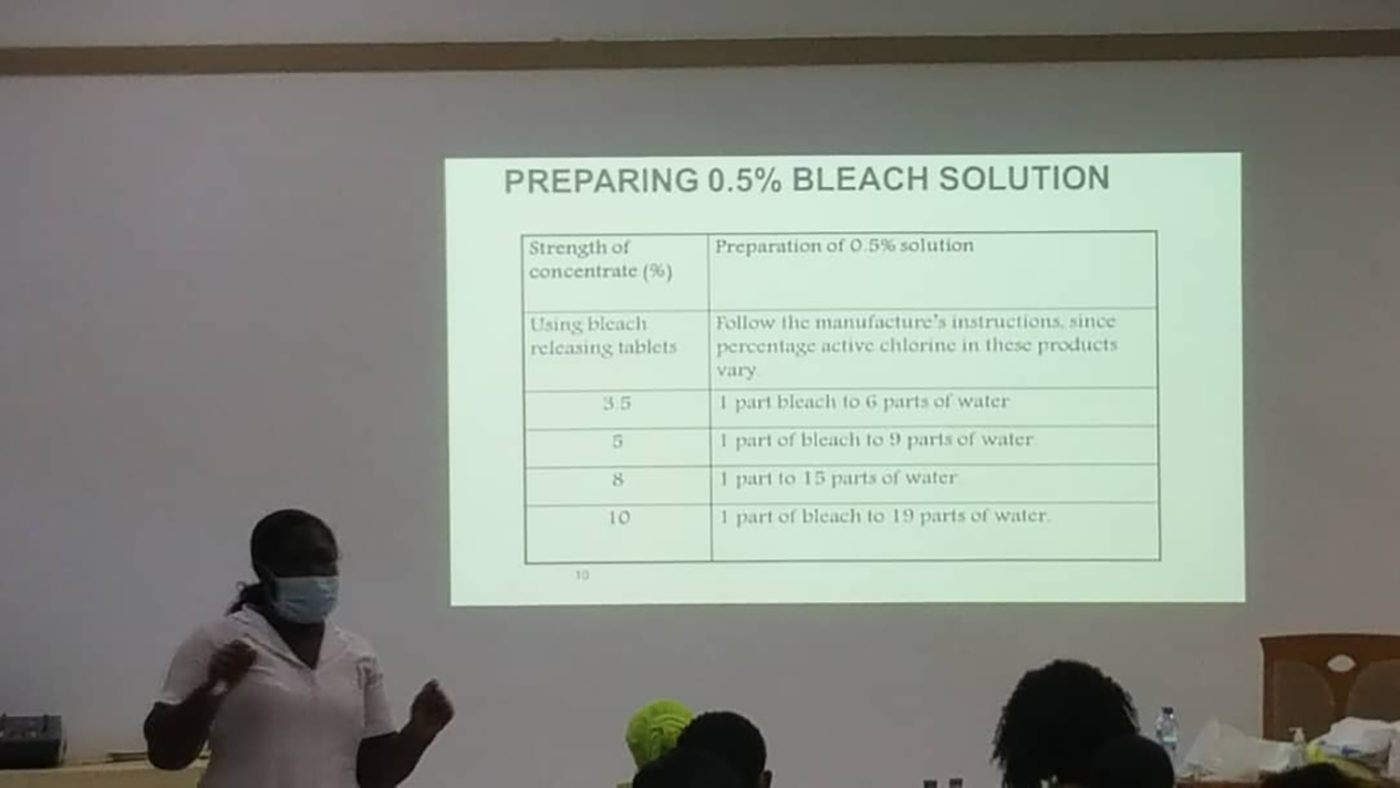
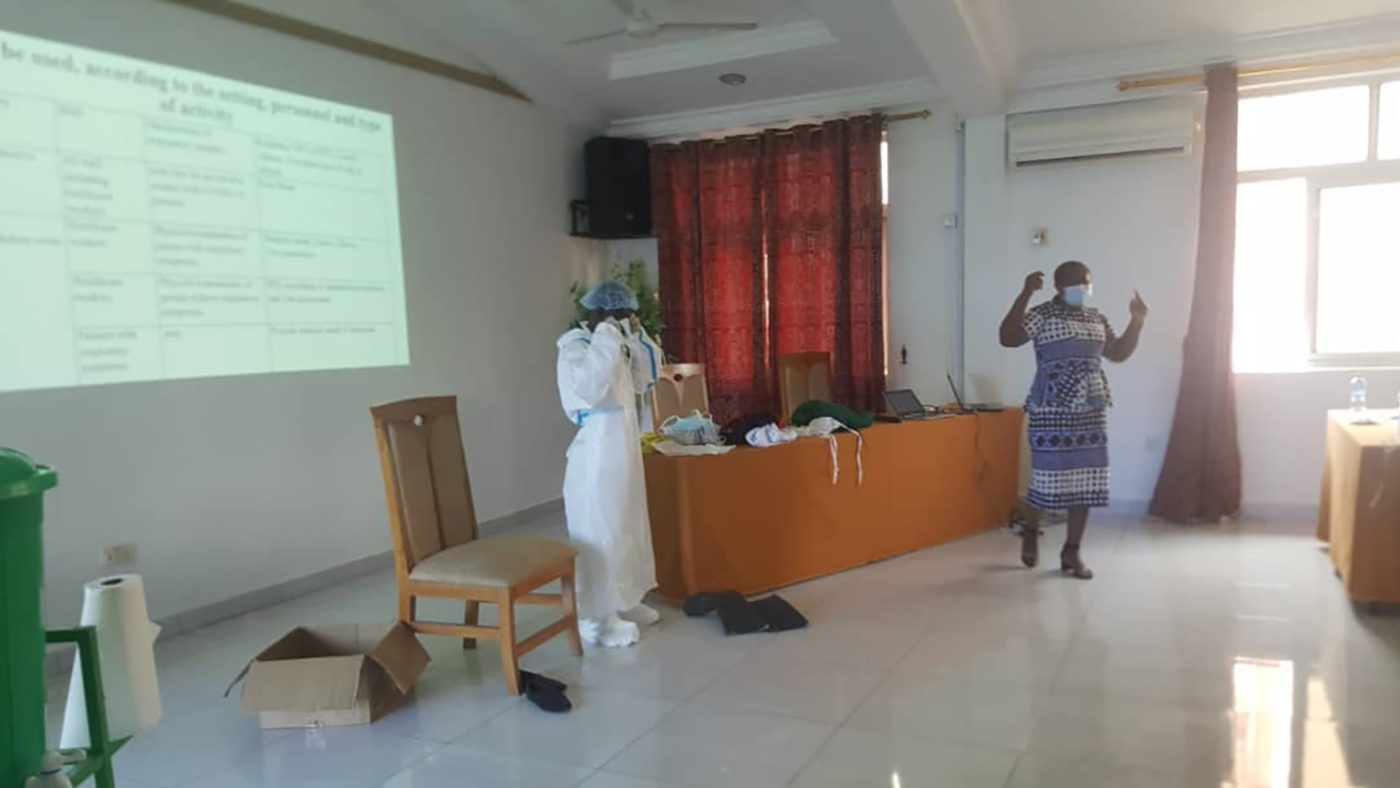
“We’ve been helping to train local volunteers, including nurses, midwives, laboratory technicians, school health coordinators and doctors’ assistants, in contact tracing, infection prevention control, risk communication and enhanced surveillance for COVID-19. They also learned to put on PPE safely, the importance of hand washing, and how to prevent and control infections. This shows how our strong relationships with partners, and our work to strengthen health systems, has enabled us to train people in the midst of the pandemic without being physically present.” More from Ghana


Syeda Asma Rashida, senior programme officer in Bangladesh
“We usually support about 50,000 operations every year, but COVID-19 has forced thousands of critical cataract operations to be cancelled, which leaves many people in an even more vulnerable situation. Bangladesh has one of the highest rates of untreated cataracts in the world, so we always have a long list of patients needing surgery. Because of COVID-19, that backlog has grown even larger.
“Through our Right to Health project, we are advising hospitals on hygiene measures, such as installing wash basins outside the entrances and cleaning more frequently, to ensure our programmes can restart safely.
“Our patient screening eye camps have had to stop. However, staff at our partner hospitals are communicating with patients by phone and telling them the extra precautions being taken: additional cleaning, as well as using sanitiser and PPE, to make the hospital safe. They are helping patients not to fear the hospitals and the response has been really good.
“We’re also making sure staff at our partner hospitals are supported. We’re happy that hospitals have taken our advice and are rotating staff so that fewer need to be working at the same time. We are also making sure older staff or those more at risk of COVID-19 do not need to go into work.” More from Bangladesh
Andre Saturnin Cossi Ridagba, programme officer in Benin
“In Benin, life is relatively normal. We do not claim to have defeated COVID-19, but government measures have been working.
“To continue our work to eliminate neglected tropical diseases, we have introduced COVID-19 measures such as a COVID-19 prevention checklist, social distancing, use of PPE and useful contacts. We’ve shared these measures through workshops with everyone involved, including the ministry of health. Thanks to their success, we are able to resume our work. At the end of October, we plan to carry out operations for people with advanced stages of trachoma in five districts.
“I hope for good days for eye health in Benin: the elimination of trachoma depends on a good eye health system, which we’re working to create.” More from Benin
Barbara Anang Marok, eye health project officer in Nigeria
“Weve helped to reopen one of the eye clinics we work with, and helped them provide personal protective equipment to minimise the spread of COVID-19. The clinic is performing operations for children who have developed cataracts because of trauma.
“One person who has received treatment at the reopened clinic is nine-year-old Destiny George, who was injured with a hockey stick. His right eye went red and would stream constantly and after a couple of weeks his eye turned white, and his mother Lovina was very concerned. He needed surgery, which usually costs NGN50,000 [about £102], otherwise he would lose his sight. Lovina didn’t have this money but the treatment was free.
“We’ve also developed accident prevention messages to be aired on the radio, highlighting the need for children to avoid using potentially harmful objects while playing. This is really important because children are spending more time at home while schools are closed.
“We have adapted our neglected tropical disease programme to ensure people in Nigeria are treated and prevented from getting trachoma. We’ve adapted the trachoma programme, training local volunteers go from house to house to distribute medicine rather than distributing to large groups in a central location.” More from Nigeria


Find out more about our work
World Sight DayOur work during COVID-19

COVID-19 prevention messaging to reach millions in Africa
Sightsavers has joined forces with M&C Saatchi World Services to produce new COVID-19 awareness campaigns that will reach millions of people.

Programme staff explain how we’re supporting children's learning during lockdown
Sightsavers staff provide a first-hand insight into the five ways we’re making sure children with disabilities aren’t left behind during the COVID-19 pandemic.

Providing trachoma treatment during lockdown in Nigeria
Dozens of people have received vital post-operative treatment for trachoma despite COVID-19 restrictions, thanks to eye surgeon Kabir Yahaya.

Saving sight in Senegal during the COVID-19 pandemic
Without eye surgeon Babacar's efforts, people could have been at risk of going blind from the advanced form of trachoma during the lockdown.

COVID-19: updates from around the world
Find out how our staff and partners in Bangladesh, Nigeria, India and Senegal are adapting amid the COVID-19 crisis.

Supporting people with disabilities in India during COVID-19
Sightsavers staff around India are making sure that during the pandemic, nobody should be excluded because of disability or gender.





