‘Prevention is better than cure’: How social behaviour change prevents glaucoma blindness
As the saying goes, ‘prevention is better than cure’ and prevention is key to addressing glaucoma, as early treatment can prevent further sight loss. Changing social behaviour could be the solution to the problem of many people losing their sight due to glaucoma.
The Keep Sight initiative launched in Nigeria in October 2019, as a collaboration between Sightsavers, Allergan and the International Agency for the Prevention of Blindness (IAPB).
Through the initiative, we are exploring specific strategies that will inform and encourage people who are at risk of glaucoma (such as people over the age of 40 who have a family member with glaucoma or who have lost their sight) to attend eye screenings. The initiative also supports people who have a diagnosis of glaucoma to cope with their chosen treatment, as the condition often requires lifelong management.
Some of the factors that affect people’s behaviour and their decision to seek treatment can be seen in Emeka’s story.

What is the Keep Sight initiative?
Keep Sight launched in 2019, and aims to treat and prevent glaucoma in India and Nigeria,
About the initiative
Emeka’s story
Emeka is 54 years old and lives in Abuja, Nigeria. His treatment journey started when he was diagnosed with glaucoma more than three years ago.
Although Emeka’s vision had been gradually deteriorating, he was unaware he had glaucoma until one morning he woke up with blurred vision. Some people believe that being visually impaired is a normal part of the ageing process, so they don’t seek help for their sight loss. This is one of the main barriers that the Keep Sight project identified in its analysis, and one of the largest obstacles to overcome.
Symptoms of glaucoma don’t appear straight away, which means that often by the time the condition is diagnosed it is advanced. Early detection is key to reducing the number of people going blind from glaucoma.
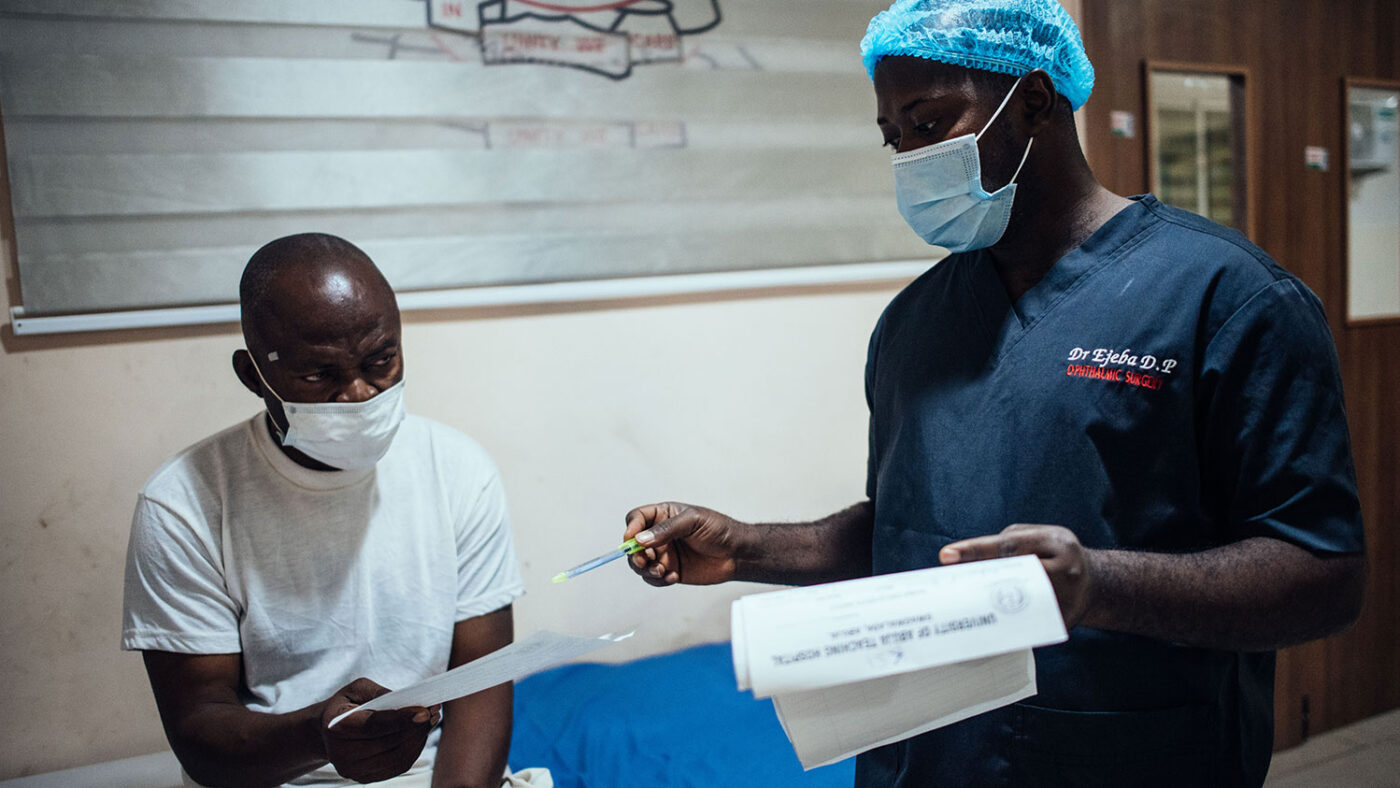
One of the barriers Emeka faced was that he was not aware of the disease. It took many visits to the hospital for him to be convinced that he needed treatment as he had not previously heard about glaucoma. The experience that patients have at health care centres is also important. Patients are more likely to continue with their treatment if they feel welcomed by staff, receive good counselling and feel that the hospital is efficiently run.
After understanding the seriousness of glaucoma and its impact, Emeka was committed to his treatment. He was given eye drops, which he used twice a day, for three years. He felt comfortable using them and did not experience any adverse effects. Despite the eye drops, his vision worsened, and he eventually had surgery on his right eye.
Another barrier that was examined was the cost of treatment. A comprehensive eye test costs about 15,700 NGN (about £30) and surgery costs 40,000 NGN (£76). Emeka had been struggling to keep up with payments for his treatment and could not afford the surgery, so the Keep Sight project paid to reduce his financial burden.
Before his surgery, Emeka said: “I feel happy because at least it will reduce part of the problem for me. From what I was told, I have confidence that after the surgery, I will be able to at least manage the problem and accept it in a way that I can take care of it.”
“I have confidence that after the surgery, I will be able to at least manage the problem and accept it in a way that I can take care of it”
Why is social behaviour change important for tackling glaucoma?
From the formative behavioural analysis, we now understood some of the enablers and barriers to people attending an eye examination and seeking treatment for glaucoma. These lessons then helped us to develop future interventions.
Social behaviour change can potentially lead to improved eye health as it can increase attendance to screenings and encourage people to adhere to their required treatment. Social behaviour change strategies can empower individuals and their families who are at risk to take control over decisions and greatly improve their eye health outcomes.
To enable us to develop the right social behaviour change plan for adults at risk of glaucoma, we identified four behaviours to focus on:
- Attending an eye screening at the primary health centre in Dobi community
- Attending hospital testing after being referred from the primary health centre
- Adhering to treatment after being diagnosed with glaucoma at hospital
- Attending routine hospital appointments as prescribed by ophthalmologists
How do these behaviours affect the patient’s journey?
Attending an eye screening, the first behaviour, is key in the patient’s journey and was especially so for Emeka. He only attended a screening after experiencing a severe symptom and a key element of the Keep Sight initiative is to support people to not be driven by their symptoms. To increase attendance, the project is planning sensitisation and enlightenment activities, and producing communication materials to enhance knowledge on how to protect eyesight, even if the patient is not aware of a problem. The project will also be promoting a culture of attending regular eye checks for at-risk individuals and will hold glaucoma awareness sessions, retrain community volunteers to persuade people, and share success stories of early detection.
The next step in a patient’s journey is to attend hospital testing when they’ve been referred. Emeka visited the hospital many times and needed to be convinced about the effects of glaucoma. This is only possible when health care workers support patients and are empathetic with their needs and concerns. Keep Sight is looking to hold interactive sessions with health care workers to discuss the impact of their actions and give advice on how to be more supportive.
To ensure patients adhere to treatment, the Keep Sight project is planning sensitisation sessions to make sure patients are informed about the importance of maintaining their treatment schedule. Support groups will also be formed so patients can encourage and motivate each other, and the project will work to enrol patients on the National Health Insurance Scheme (NHIS).
The final behaviour aims to help patients understand the severity of glaucoma so that they are committed to attending their regular appointments. Emeka was committed to his treatment due to his understanding of its importance and was also accepting of surgery as it would help him manage his glaucoma. The Keep Sight project will work to improve the uptake of surgery by holding awareness events, organising individual and group counselling sessions, producing social behaviour change materials to encourage acceptance of surgery, and distributing positive testimonials about surgery.
Emeka’s experience outlines just some of the key insights that have been learnt from the Keep Sight project. The formative behavioural analysis summary and report lay out the above enablers and barriers in more detail alongside other insights.

What’s next?
From the formative behavioural analysis, Sightsavers and the Keep Sight initiative are developing specific activities, messages and materials that are tailored to the community. These will not necessarily provide information but aim to boost the confidence of individuals in the community to make the right decisions about their eye health, attend an eye screening or adhere to their treatment plan.
We are also looking to the future to make sure people do not wait for their glaucoma to become severe before they accept treatment. By using the right social behaviour change plan, we can reduce the number of people going blind due to untreated glaucoma. The initiative found that making people take early responsibility for their eye health was the most effective route. Simply, a stitch in time saves nine.
Author
 Selben Penzin is a senior programme manager for eye health at Sightsavers and is based in Nigeria.
Selben Penzin is a senior programme manager for eye health at Sightsavers and is based in Nigeria.
Want to learn more about our work?
About SightsaversMore blogs

Why community collaboration is important in our research
Our research on female genital schistosomiasis has highlighted the need to establish a safe and supportive environment for participants when studying sensitive topics.

The key to inclusive education is engaging organisations of people with disabilities
Collaborating with organisations of people with disabilities (OPDs) on our inclusive education projects has earned the Sightsavers-led Inclusive Futures consortium a Zero Project Award in 2024.

Six takeaways from the International Conference for Public Health in Africa
Sightsavers’ Hortance Manjo shares insights from the event in Zambia, which highlighted eye health for the first time.